SOAP Notes 2014-2026 free printable template
Show details
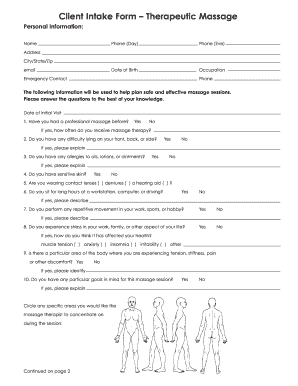
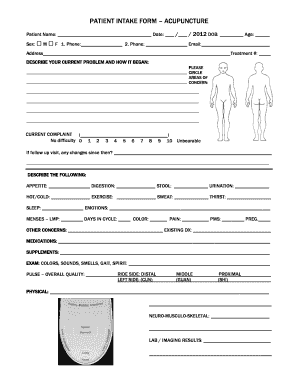
SOAP Notes Patient Name or Inflammation Rotation Long Tender Point Trigger Point Elevation Inflammation Rotation
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign soap notes for massage therapy form

Edit your massage therapy soap notes templates form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.

Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.

Share your form instantly
Email, fax, or share your printable soap note template form via URL. You can also download, print, or export forms to your preferred cloud storage service.
How to edit massage soap notes template online
Use the instructions below to start using our professional PDF editor:
1
Log in to account. Start Free Trial and register a profile if you don't have one yet.
2
Simply add a document. Select Add New from your Dashboard and import a file into the system by uploading it from your device or importing it via the cloud, online, or internal mail. Then click Begin editing.
3
Edit soap notes form. Rearrange and rotate pages, add and edit text, and use additional tools. To save changes and return to your Dashboard, click Done. The Documents tab allows you to merge, divide, lock, or unlock files.
4
Get your file. Select your file from the documents list and pick your export method. You may save it as a PDF, email it, or upload it to the cloud.
It's easier to work with documents with pdfFiller than you can have believed. Sign up for a free account to view.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
SOAP Notes Form Versions
Version
Form Popularity
Fillable & printabley
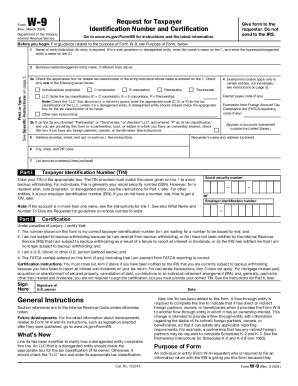
How to fill out printable soap note template pdf form

How to fill out printable soap notes:
01
Start by gathering all the necessary patient information, including their name, age, and contact information.
02
Record the date and time of the patient encounter at the top of the SOAP note.
03
Begin with the "Subjective" section, where you document the patient's chief complaint and any relevant medical history or symptoms they are experiencing.
04
Move on to the "Objective" section, where you record the findings from the physical examination, diagnostic tests, and any other objective data.
05
In the "Assessment" section, provide a diagnosis or list of differential diagnoses based on the subjective and objective information.
06
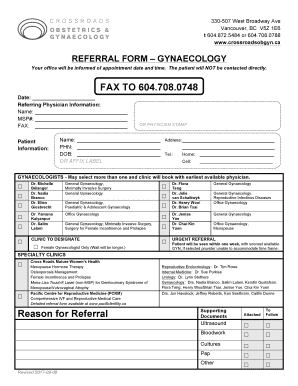
Create a plan of care in the "Plan" section, outlining the treatments, medications, referrals, or any other interventions recommended for the patient.
07
Make sure to include any follow-up appointments or instructions for the patient in the "Plan" section as well.
08
Sign and date the SOAP note to indicate the healthcare provider who completed it.
09
Keep the SOAP notes organized and in a secure location for future reference.
Who needs printable soap notes:
01
Healthcare providers, including doctors, nurses, and therapists, use printable SOAP notes to document patient encounters and track the progress of their care.
02
Medical students and residents may also use printable SOAP notes as a learning tool to practice their documentation skills and develop their clinical reasoning abilities.
03
Other healthcare professionals, such as chiropractors, physical therapists, and psychologists, may also utilize printable SOAP notes in their respective fields to keep track of patient information and treatment plans.
Fill
blank soap note template
: Try Risk Free






People Also Ask about soap notes template
How do you structure a SOAP note?
The 4 headings of a SOAP note are Subjective, Objective, Assessment and Plan.
What is SOAP note template?
SOAP—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way.
How do you write a simple SOAP note?
SOAP notes include a statement about relevant client behaviors or status (Subjective), observable, quantifiable, and measurable data (Objective), analysis of the information given by the client (Assessment), and an outline of the next course of action (Planning).
What is a SOAP note and how is it structured?
In modern clinical practice, doctors share medical information primarily via oral presentations and written progress notes, which include histories, physicals and SOAP notes. SOAP—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way.
What does a good SOAP note look like?
SOAP notes include a statement about relevant client behaviors or status (Subjective), observable, quantifiable, and measurable data (Objective), analysis of the information given by the client (Assessment), and an outline of the next course of action (Planning).
How do you write a SOAP note template?
SOAP Note Template Document patient information such as complaint, symptoms and medical history. Take photos of identified problems in performing clinical observations. Conduct an assessment based on the patient information provided on the subjective and objective sections. Create a treatment plan.
Our user reviews speak for themselves
Read more or give pdfFiller a try to experience the benefits for yourself
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I complete massage soap note template online?
Completing and signing soap note template pdf online is easy with pdfFiller. It enables you to edit original PDF content, highlight, blackout, erase and type text anywhere on a page, legally eSign your form, and much more. Create your free account and manage professional documents on the web.
Can I edit printable soap notes for massage therapy on an iOS device?
Create, edit, and share massage soap notes form from your iOS smartphone with the pdfFiller mobile app. Installing it from the Apple Store takes only a few seconds. You may take advantage of a free trial and select a subscription that meets your needs.
How do I fill out printable blank soap note template pdf on an Android device?
Use the pdfFiller Android app to finish your massage soap notes pdf and other documents on your Android phone. The app has all the features you need to manage your documents, like editing content, eSigning, annotating, sharing files, and more. At any time, as long as there is an internet connection.
What is SOAP Notes?
SOAP Notes are a structured method of documentation used by healthcare providers to record patient progress and treatment plans, consisting of four components: Subjective, Objective, Assessment, and Plan.
Who is required to file SOAP Notes?
Healthcare professionals such as doctors, nurses, therapists, and other clinicians involved in patient care are required to file SOAP Notes as part of their clinical documentation.
How to fill out SOAP Notes?
To fill out SOAP Notes, practitioners should gather information for each component: Subjective (patient's statements), Objective (observations and clinical data), Assessment (diagnosis or evaluation), and Plan (treatment strategy and follow-up actions).
What is the purpose of SOAP Notes?
The purpose of SOAP Notes is to provide a clear and concise framework for documenting patient interactions, facilitating communication between providers, and ensuring continuity of care.
What information must be reported on SOAP Notes?
Information reported in SOAP Notes must include the patient's subjective complaints, objective findings, clinical assessment, and treatment plan, including any scheduled follow-ups or referrals.
Fill out your SOAP Notes online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Massage Therapy Soap Notes Templates Word is not the form you're looking for?Search for another form here.
Keywords relevant to massage therapy soap notes template
Related to digital soap notes pdf
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.